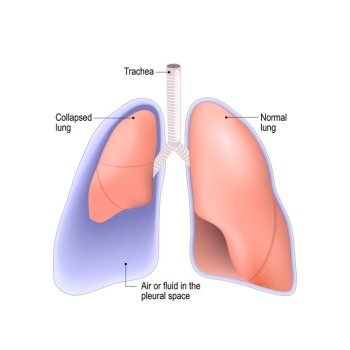
How is a collapsed lung treated? Very small lung collapses (less than 5% collapsed) require little treatment and will get better with time and rest. In most cases, a chest tube is inserted to re-expand the lung. Chest tubes remove air that has been trapped outside of the lung. Chest tubes are typically left in place for several days. If the lung does not heal from the chest tube, additional surgery is required.
Currently, there are two main types of surgical procedures used to treat a spontaneous pneumothorax: a pleurodesis (physical or chemical) and a pleurectomy. During a physical pleurodesis, the surface of the lung will be scraped to cause bleeding and scarring. Although this seems counterintuitive, the hope is that once the scar tissue heals it will prevent the lung from collapsing in the future even if new blebs develop. Any blebs found during the surgery will also be removed. It is important to realize that this does not prevent additional blebs from developing in the future. This surgery is usually conducted with a small video camera and is called VATS (Video Assisted Thoracic Surgery). The video scope is placed through a small, roughly one-inch incision while the surgeons operate their tools through few other small incisions. During a chemical pleurodesis, tetracycline or other chemicals are used to burn the surface of the lung, again in the hopes of scarring the lung so that it can no longer collapse.
After this surgery a patient may have two chest tubes to help with recovery. These tubes are attached to a machine called a Pleurovac, which helps keep the lung inflated while it heals by lightly suctioning air through the tubes. Another purpose of the chest tubes is to allow blood to drain from the chest cavity. Normally a lung will heal after about four or five days. The chest tubes will be removed at this time and the patient is free to leave the hospital. Within a month most people can return back to their normal activities. This is the normal course of a pleurodesis. If complications occur, additional procedures may be required and thus more time to heal will be needed. Patients can be incorrectly told that they are “cured” by the pleurodesis and that their lungs will not collapse again. Unfortunately this is untrue. According to a prominent thoracic surgeon from Cedars Sinai Hospital in Los Angeles, about 10% of patients who undergo a pleurodesis will eventually experience another collapsed lung.
Another surgery used to treat a collapsed lung is called a pleurectomy. This procedure has been described as “brutal” by surgeons and is only used if a patient experiences several repeat lung collapses or if other attempts to repair a lung have failed. The pleura lining of the lung is literally torn from the lung in order to produce more extensive bleeding and scarring. The hope is that this additional scarring will create an even stronger lung, thus decreasing the likelihood of future collapses if a bleb develops. This procedure is more painful than a pleurodesis and will take a longer time to heal from. Unfortunately, a lung collapse could still occur after this surgery despite being declared “cured.” While these are the two most common surgical treatments, its important to check with your surgeon about any updated treatment options.
Are patients cured after surgery?
A prominent thoracic surgeon from Cedars Sinai Hospital in Los Angeles believes that roughly 90% of patients who undergo a pleurodesis will not experience another collapsed lung. While these patients may be viewed as “cured,” they may still have to deal with chronic pain. A collapsed lung, chest tube(s), or a pleurodisis surgery can cause chronic pain. In addition, these surgeries do not prevent new blebs from developing and therefore many people still suffer from pain when new blebs rupture and leak air. Patients less fortunate will experience additional lung collapses from new blebs. Unfortunately the only treatments available at this time are the surgeries discussed above. However check with your surgeon or doctors about any updated treatments.
Once you heal from surgery, are you pain free?
Unfortunately this is highly unlikely. Understand that the surgeries cause permanent scarring and damage to some of the most sensitive tissues in the human body. Often patients experience chronic pain from the physical trauma of surgery. A study by Passlick, Born, Sienel and Thetter, published in the European Journal of Cardio-thoracic Surgery found that chronic pain was very common even after minimally invasive surgery for patients with spontaneous pneumothorax. This study followed 60 patients who underwent a VATS Pleurodesis or Pleurectomy. Five years after the surgery, 31.7% of the patients still had chronic pain. It is important to consider that in this study the patients had only undergone one surgery (2001, p. 355-359). With patients who have undergone several surgeries, their chance of experiencing chronic pain is likely even higher.
While some people may experience positive results after surgery as far as preventing their lung from collapsing, surgeries cannot remove the pain associated with blebs or pain as a result of the surgery. Often after surgery, when the lung is declared “fixed,” a patient must then learn to cope with chronic pain. They are then directed to a new team of doctors who specialize solely in pain medicine. Patients can often feel frustrated and angry once they realize the surgery has left them with a whole new problem requiring a new team of doctors, treatment, medicines and direction. The chronic pain can be so severe that it can greatly limit a patient’s quality of life.
How can blebs be treated?
Blebs can be very painful even if they do not cause a collapse. Many patients will experience “unexplained pain” caused by blebs which do not always show up on an x-ray. Even if a doctor is able to determine that there are leaking blebs, nothing can be done. Surgery is only warranted when the lung collapses. Thus, a patient must simply wait patiently. A leaking bleb will either heal or unfortunately grow larger and cause the lung to collapse, then requiring surgery. Patients in this scenario are often greatly limited by pain.
Why should I consider therapy if I have bleb disease?
Going to counseling will not fix your bleb disease. However therapy can help you cope with having bleb disease. Sometimes the experience of having a collapsed lung and undergoing the medical treatment required can be traumatizing. It is helpful to process these experiences with a therapist, especially if you continue to need medical treatment. A therapist can also help you with the grieving process around losses you have experienced due to bleb disease. It is important to know that people with chronic pain often experience depression. If you experience chronic pain due to bleb disease and/or the treatment of bleb disease consider seeking therapy to help you cope with the chronic pain and any accompanying depression. Therapy can also help you negotiate role shifts you may be experiencing due to new limitations. Learning how to more effectively manage your stress is another benefit of going to therapy.












